Palliative mouth care
Mouth problems are common in palliative care and during end of life. Good oral hygiene is important for everyone, especially during illness when it can help prevent mouth problems from developing, such as tooth decay, tooth loss, a dry mouth, bleeding gums, gum disease, and halitosis.
Palliative mouth care will be offered to you or your family member at each visit from our Hospice at Home team, but it is also something that can be done throughout the day as necessary or desired. Please download our resource below for an overview on some basic principles on how to provide good oral hygiene and why it is important.
Introduction
This guide has been written by Dorothy House Hospice at Home care staff who have a special interest in mouth care. Mouth care is essentially caring for oral hygiene and includes the assessment and cleaning of teeth/dentures, gums, tongue, roof of the mouth and lips.
Mouth care will be offered to you or your family member at each visit from our Hospice at Home team, but it is also something that can be done throughout the day as necessary or desired. We have set out some basic principles on how to provide good mouth care and why it is important.
We also describe some common mouth problems and tips on how to keep the mouth feeling moist, clean and comfortable.
Why mouth care matters
Self-care
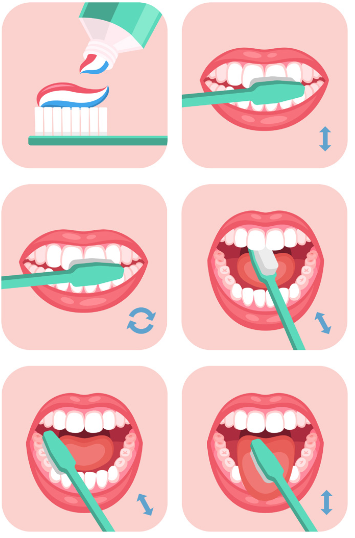
Good oral hygiene is important for everyone, especially during illness when it can help prevent mouth problems from developing. The effects of poor oral hygiene may include tooth decay, tooth loss, a dry mouth, bleeding gums, gum disease, and halitosis. It is recommended that teeth are brushed twice a day using a soft toothbrush and fluoride-containing toothpaste. Official advice is not to rinse after brushing, as the fluoride from the toothpaste stays on the teeth longer, helping to decrease the likelihood of decay.
Please continue to brush your teeth if you are able to. Hospice at Home carers will offer assistance and will be happy to show your family members how they can help too.
- Some people find that rinsing the mouth with warm water after meals and at night can be soothing.
- Unless mouthwash has been advised by a dental professional, it is best avoided. Many mouthwashes contain alcohol which can cause mouth dryness or stinging.
- Dentures should be cleaned with a soft toothbrush and liquid soap or denture toothpaste (normal toothpaste is too abrasive and can damage dentures over time). Some people find it helpful to clean dentures over something soft like a folded towel, to prevent breakages if they are dropped. Soak dentures in denturecleaning solution for the required time (follow the manufacturer’s instructions), and rinse in running water before returning to the mouth. Try to ensure that dentures are fitting properly as a poor fit can cause soreness to the mouth and gums. Dentures can lose their shape if they are not kept moist, so it is best to keep them in water in a suitable container overnight – for gum health it is not recommended to wear dentures overnight.
Some common problems
Some common problems
Drink adequate fluids, especially water. Fizzy drinks are best avoided as they may sting.
- Try drinking through a straw.
- Taking frequent sips of water can help keep the mouth moist – keep a glass of water by the bed.
- Try sucking ice cubes or ice lollies – fruit juices can also be frozen in ice cube trays.
- Sugar-free chewing gum can sometimes help to produce more saliva, also sugarfree boiled sweets, pastilles and mints.
- Use a mild, non-foaming toothpaste for teeth cleaning.
- Avoid alcohol as it can irritate the mouth.
- Avoid smoking as it can also irritate the mouth.
- Caffeinated or citrus drinks may also irritate the mouth.
- Try a moisturising mouth gel, for example, Oralieve (no prescription is needed).
- Tell your dentist, doctor, district nurse or nurse specialist about a dry mouth – they can prescribe mouthwashes, lozenges, artificial saliva sprays, or tablets if required.
- Use a lip balm to protect the lips (for example Vaseline). However, if oxygen is being used, apply a water-soluble lubricant instead.
- Certain drugs like opioids (for example, morphine) can increase mouth dryness.
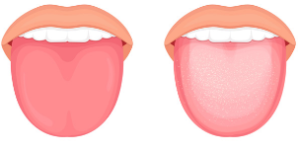
If your tongue is coated or furred
- This may make food taste unpleasant and put you off eating.
- The tongue can be cleaned with a bicarbonate of soda solution – dissolve 1 teaspoon of bicarbonate of soda (available from supermarkets and chemists) in a pint of warm water. Use a small, soft toothbrush or gauze dipped in the solution to clean the tongue.
- If this does not help, talk to your dentist, doctor, district nurse or nurse specialist who can give more advice because it could be oral thrush. Thrush coats the tongue, the inside of the cheeks and the back of the throat – it may look red with spotty or pale patches. Drugs such as steroids and antibiotics can increase the risk of oral thrush.
Normal and white coated tongue
Oral thrush
© James Heilman
Halitosis (bad breath)
- Regular oral hygiene, including tongue cleaning, and good care of dentures is important.
- Adequate fluid intake, especially water, may help – take small sips regularly throughout the day.
- Avoid smoking.
- Some mouthwashes may reduce breath odour, but avoid those containing alcohol.
Mouth ulcers
- May be painful and make eating and drinking difficult.
- Avoid acidic, spicy or salty food and very hot or acidic drinks.
- Try drinking cool drinks through a straw.
- Salt mouthwashes or anti-inflammatory mouthwashes, such as Difflam, can help relieve pain. You can buy pain relieving gels, for example Bonjela, without a prescription.
- Speak to your dentist, doctor, district nurse or nurse specialist if mouth ulcers last longer than 2 weeks, or if they bleed or become more painful.
Maksim, 11 September 2016
Dry, cracked or bleeding lips
- Use a lip balm such as Vaseline to help keep the lips moist and comfortable. If oxygen is used however, remember that Vaseline cannot be used – try a water-based lubricant instead.
Changes in taste
Some treatments can affect the way food tastes. Taste changes are a common side effect of chemotherapy – this usually stops about 3 to 4 weeks after treatment ends. Radiotherapy can also cause taste changes which usually start to improve 3 weeks to 2 months after treatment ends. Other medicines such as morphine and antibiotics can cause taste changes too.
- Try different foods to see which taste best to you.
- Try bland foods such as bread, potatoes and crackers. Alternatively, try using seasonings, spices and herbs to add more flavour.
- Sharp-tasting foods, such as fresh fruit, fruit juices and sugar-free sour or boiled sweets, can be refreshing and leave a pleasant taste in the mouth.
- If you no longer like tea or coffee, try lemon tea, herbal teas or cold drinks such as lemonade (sugar-free is best).
- Some people find cold foods taste better than hot foods.
- Brush your teeth before meals
If a person is unable to care for their own mouth:
- Ask how their mouth feels and check on the condition daily – a small torch can be useful to help inspect the mouth.
- Mouth care is best performed when the patient is sitting up, or with their head elevated.
- Remember to wash your hands or wear gloves.
- Try to offer mouth care every 1-2 hours if possible, as this will help hydrate the mouth and maintain comfort. This is especially important if someone is not able to eat or drink anything anymore, if oxygen is used, or if they are sleeping more.
- Use a soft toothbrush dipped in fresh water – you can buy toothbrushes suitable for babies as they are smaller and softer and are less likely to damage the mouth. We can sometimes provide a 360º toothbrush.

- Do not leave a toothbrush in water ready for next time as this can harbour bacteria – dry the toothbrush and use fresh water each time.
- Pink sponges on sticks are no longer recommended for mouth care as they can cause choking if they become detached in the mouth.
- Consider ‘taste for pleasure’ after you have given mouth care. A soft toothbrush can be dipped into the person’s favourite flavour drink to provide enjoyment and to offer some moisture. After dipping the brush into the drink, shake off any excess and use around the lips and then inside the mouth.
- Ask your Hospice at Home carers for advice – we will be happy to show you how you can help your loved one maintain a clean and comfortable mouth.
References
Mouth problems and cancer treatments.
Macmillan cancer support – https://www.macmillan.org.uk/cancer-information-andsupport/impacts-of-cancer/mouth-problems
Mouth Care Matters – elearning for health. https://www.e-lfh.org.uk
Palliative care – oral. NICE (National Institute for Health and Care Excellence). https://www.cks.nice.org.uk
Mouth care matters in end of life care. Royal College of Nursing. https://www.rcn.org/magazines
NHS Health A to Z. Dentures (false teeth) https://www.nhs.uk/conditions/dentures/
The Palliative Care Handbook. A Good Practice Guide. Wessex Palliative Physicians. Ninth edition (2019) – https://www.ruh.nhs.uk/for_clinicians/departments_ruh/palliative_care/documents/palliative_care_handbook.pdf