Pressure ulcers
Pressure ulcers, also known as bed sores or pressure sores, are areas of damage to the skin and underlying tissue. They can develop anywhere on the body but are mostly found over bony areas such as heels, elbows, hips, bottom, spine and ankles. Skin damage results from the weight of the body pressing down on an areas of skin for too longs without relief.
The following downloadable resource covers areas of preventing and managing pressure ulcers, such as where they can develop on parts of the body, how to spot early signs, and how to reduce the risk of pressure damage.
Pressure ulcers, also known as bed sores or pressure sores, are areas of damage to the skin and underlying tissue.
What causes a pressure ulcer?
Skin damage results from the weight of the body pressing down on an area of skin for too long without relief. Lying in one position for too long can cause this. This reduces blood supply to the area which may appear as a red area, blister or an open wound.
Shearing force can also cause skin damage. This is when layers of skin are forced to slide over one another, for example, when you slide down or are pulled up in a bed or chair.
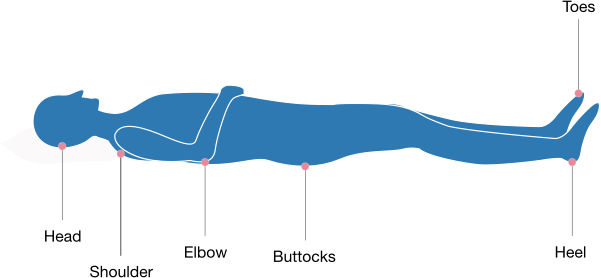
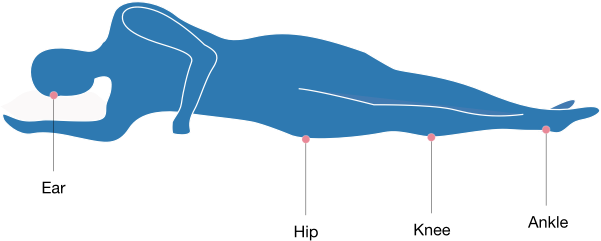
What parts of the body can get a pressure ulcer?
Pressure ulcers can develop anywhere on the body but are mostly found over bony areas such as heels, elbows, hips, bottom, spine and ankles.
What you can do to help reduce the risk of pressure damage
Keep moving
Changing your position regularly, whether you are in a bed or in a chair, helps relieve pressure.
If you are in bed, try changing sides regularly, sit up slightly and use the flat of your foot and not your heel to push you up the bed. If you have difficulty moving or changing your position alone, your carer or nurse will be able to help you. We appreciate that you may not wish to be repositioned regularly, but it is very important to do this to reduce the possibility of pressure damage occurring.
Nutrition
Eating a nutritious diet will keep your skin in good condition and you should drink plenty of fluids.
Skin inspection
Check your skin for signs of early damage as this will allow action to be taken to prevent a pressure ulcer from developing. Be aware of your skin’s normal colour, texture and temperature. Always check areas you lie on or ask others to check for you.
Skin care
Keep skin clean and dry. Wash skin daily. If your skin requires more frequent washing, for example due to incontinence, use a soap substitute to prevent stripping the skin of its natural protective oils.
Incontinence
If incontinence is a problem, this can increase your risk of pressure ulcers as your skin will be more vulnerable to damage. The use of pads to contain this may help. Seek advice from a health professional.
Who is most at risk of developing pressure ulcers?
You may be at risk of developing pressure ulcers for a number of reasons including:
- Difficulty changing position and poor mobility
- Poor circulation, vascular disease, diabetes or heavy smoking may affect circulation
- Reduced body sensation. Some conditions (e.g. diabetes, strokes, spinal injuries) may reduce sensitivity to discomfort or pain
- Poor nutritional status/reduced appetite and weight loss
- Presence of moisture. Urine, faeces and sweat can irritate the skin, causing it to break down more easily
- Certain medication can affect the integrity of skin (e.g. steroids)
- Early signs of a pressure ulcer
You may be at risk of developing pressure ulcers for a number of reasons including:
- A hard, swollen, warm area
- Broken skin/an open wound/blister
- Pain/discomfort
It is normal for a red mark to appear on the skin following pressure. Within 20 minutes of pressure relief this should disappear. If after 20 minutes the skin marking does not disappear this may indicate pressure damage. Those patients with darkly pigmented skin may develop a purple/blue patch.